Fundoplication: Understanding the Surgical Procedure to Treat Acid Reflux
Acid reflux, often characterized by heartburn, regurgitation, and discomfort, is a common gastrointestinal condition affecting millions worldwide. While lifestyle changes and medication can alleviate symptoms for many, some cases require surgical intervention. Fundoplication stands as a highly effective surgical procedure aimed at resolving chronic acid reflux by addressing the underlying anatomical issues. This comprehensive exploration delves into the intricacies of fundoplication, shedding light on its indications, techniques, outcomes, and potential complications.
Understanding Acid Reflux:
Before delving into fundoplication, comprehending the mechanisms of acid reflux is paramount. Normally, a muscular valve known as the lower esophageal sphincter (LES) prevents stomach contents from flowing back into the esophagus. However, in individuals with acid reflux, this valve weakens or relaxes inappropriately, allowing stomach acid and digestive juices to reflux into the esophagus, leading to irritation, inflammation, and discomfort.
Indications for Fundoplication:
Fundoplication becomes a consideration when conservative treatments such as lifestyle modifications and medications fail to provide sufficient relief. Candidates for fundoplication typically experience severe or persistent symptoms of acid reflux, such as chronic heartburn, regurgitation, difficulty swallowing, or complications like esophagitis, Barrett's esophagus, or strictures.
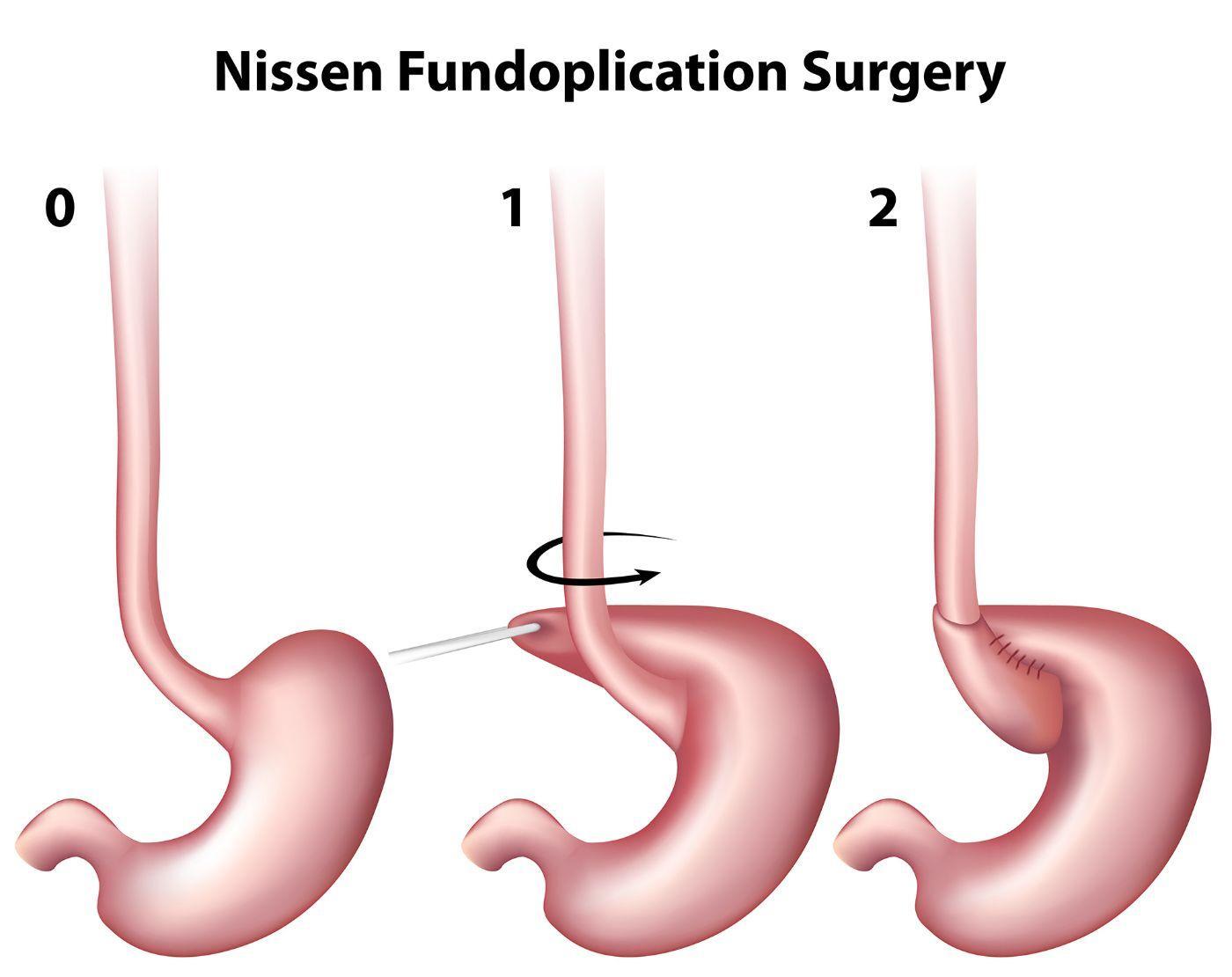
The Fundoplication Procedure:
Fundoplication is a surgical procedure performed under general anesthesia. It involves wrapping the upper portion of the stomach (the fundus) around the lower esophagus to reinforce the weakened LES, thus preventing reflux. There are two primary techniques: laparoscopic (minimally invasive) and open surgery.
Laparoscopic Fundoplication:
In laparoscopic fundoplication, surgeons make several small incisions in the abdomen through which specialized instruments and a tiny camera (laparoscope) are inserted. The surgeon then manipulates these instruments to perform the procedure while viewing the operative field on a monitor. Laparoscopic techniques offer advantages such as reduced postoperative pain, shorter hospital stays, quicker recovery times, and decreased risk of complications compared to traditional open surgery.
Open Fundoplication:
Open fundoplication involves making a larger incision in the abdomen to access the surgical site directly. While it allows for more extensive visualization and manipulation, it typically entails a longer recovery period and increased postoperative pain compared to laparoscopic approaches. However, open surgery may be necessary in cases where laparoscopic techniques are not feasible or appropriate.
Types of Fundoplication:
Several variations of fundoplication exist, including:
- Nissen fundoplication: The most common type, where the fundus is wrapped around the esophagus 360 degrees.
- Partial fundoplication (e.g., Toupet or Dor fundoplication): Involves a partial wrap around the esophagus to prevent reflux while preserving some degree of gastric emptying and reducing the risk of postoperative dysphagia (difficulty swallowing).
Outcomes and Recovery:
The success rates of fundoplication are generally high, with a significant reduction in reflux symptoms reported in the majority of patients. However, as with any surgical procedure, there are risks and potential complications, including difficulty swallowing, bloating, gas, persistent reflux, and rarely, complications related to anesthesia or surgical technique.
Postoperative Care:
Following fundoplication, patients typically remain in the hospital for observation and pain management. They may gradually resume a diet, starting with clear liquids and advancing to solid foods as tolerated. It's essential to follow postoperative instructions provided by the surgical team, including dietary recommendations, activity restrictions, and medication management.
Long-term Management:
While fundoplication can provide long-term relief for many individuals with acid reflux, ongoing management is crucial. This may include lifestyle modifications (e.g., avoiding trigger foods, maintaining a healthy weight) and continued use of medications as prescribed. Regular follow-up appointments with a healthcare provider are essential to monitor symptoms, assess for complications, and adjust treatment as needed.
Conclusion
Fundoplication remains a cornerstone in the surgical management of acid reflux, offering significant relief for individuals with persistent symptoms refractory to conservative measures. By addressing the underlying anatomical defects contributing to reflux, fundoplication can provide lasting improvements in quality of life for many patients, albeit with careful consideration of potential risks and benefits. As with any medical intervention, a thorough discussion with a healthcare provider is essential to determine the most appropriate treatment approach based on individual needs and circumstances.
