Gastro esophageal reflux disease(GERD), Hiatal hernia , Acalasia cardia,
The human digestive system is a complex network of organs working in harmony to break down food and absorb essential nutrients. Central to this system is the esophagus, a muscular tube connecting the throat to the stomach. While the esophagus typically functions smoothly, it can be subject to various disorders that disrupt its normal operation. Among these disorders, Gastroesophageal Reflux Disease (GERD), Hiatal Hernia, and Achalasia Cardia stand out as prevalent conditions that can significantly impact an individual's quality of life.
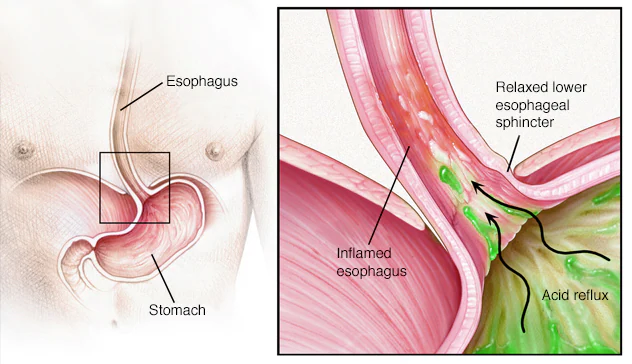
Gastroesophageal Reflux Disease (GERD)
GERD is a chronic digestive disorder characterized by the backward flow of stomach acid into the esophagus, leading to irritation and inflammation of its lining. This condition often manifests as heartburn, a burning sensation in the chest that can radiate to the throat. While occasional heartburn is common and can be managed with over-the-counter medications, persistent and severe symptoms may indicate GERD.
One of the primary contributors to GERD is the malfunction of the lower esophageal sphincter (LES), a ring of muscle at the junction of the esophagus and stomach that normally prevents stomach acid from refluxing into the esophagus. When the LES weakens or relaxes inappropriately, stomach acid can flow backward, causing irritation and discomfort.
In addition to heartburn, individuals with GERD may experience regurgitation, a sour or bitter taste in the mouth, difficulty swallowing, chronic cough, and hoarseness. Over time, untreated GERD can lead to complications such as esophagitis (inflammation of the esophagus), esophageal strictures (narrowing of the esophagus), Barrett's esophagus (a precancerous condition), and even esophageal cancer.
Treatment for GERD typically involves lifestyle modifications, such as avoiding trigger foods, losing weight, and elevating the head of the bed. Medications like proton pump inhibitors (PPIs), which reduce stomach acid production, are often prescribed to alleviate symptoms and promote healing. In severe cases or those resistant to medical therapy, surgical intervention may be necessary to reinforce the LES or correct anatomical abnormalities contributing to reflux.
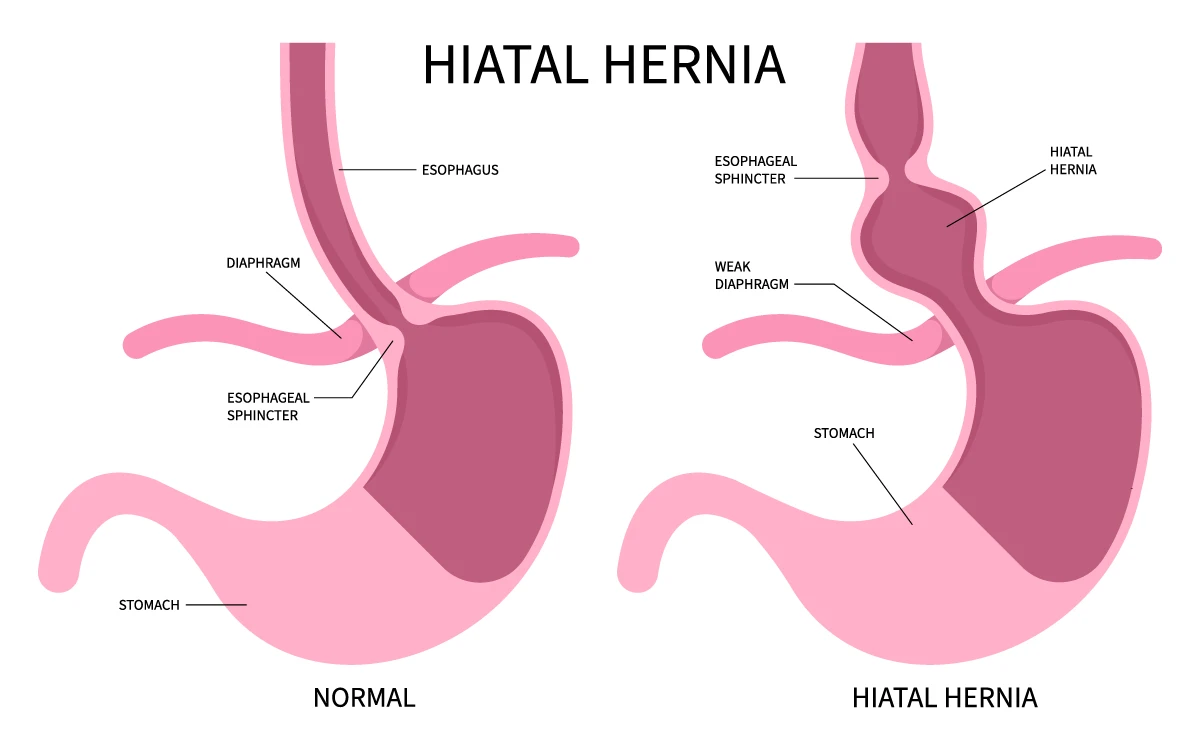
Hiatal Hernia
A hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity, typically through an opening called the esophageal hiatus. The diaphragm is a large muscle separating the chest cavity from the abdomen, and the esophageal hiatus is the opening through which the esophagus passes.
There are two main types of hiatal hernias: sliding and paraesophageal. Sliding hiatal hernias are more common and occur when the junction of the esophagus and stomach, including a portion of the stomach, slides upward into the chest. In contrast, paraesophageal hernias involve the stomach protruding through the hiatus beside the esophagus, potentially leading to complications such as strangulation or obstruction of the stomach.
Many hiatal hernias are asymptomatic and are incidentally discovered during diagnostic testing for other conditions. However, larger hernias or those associated with GERD may cause symptoms such as heartburn, regurgitation, chest pain, difficulty swallowing, and feeling full quickly after eating.
Treatment for hiatal hernias depends on the severity of symptoms and the presence of complications. Mild cases may be managed conservatively with lifestyle changes and medications to control reflux symptoms. Surgical repair, often performed laparoscopically, may be recommended for symptomatic or complicated hernias, aiming to reduce the herniated portion of the stomach and reinforce the hiatus to prevent recurrence.
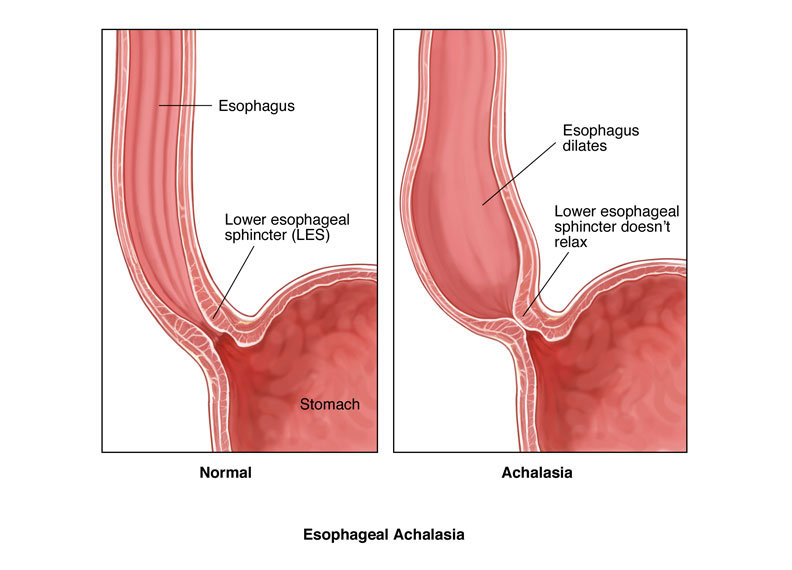
Achalasia Cardia
Achalasia cardia is a rare esophageal motility disorder characterized by the failure of the lower esophageal sphincter (LES) to relax properly during swallowing, as well as impaired peristalsis, the coordinated muscle contractions that propel food down the esophagus. This results in difficulty swallowing (dysphagia), regurgitation of undigested food, chest pain, and weight loss.
The exact cause of achalasia is not fully understood, but it is thought to involve damage or degeneration of the nerves in the esophagus responsible for coordinating muscle contractions. Genetic factors, autoimmune processes, and viral infections have been implicated in the development of achalasia.
Diagnosis of achalasia typically involves a combination of imaging studies, such as barium swallow or esophageal manometry, which measures pressure and coordination of esophageal muscle contractions. Endoscopic evaluation may also be performed to rule out other esophageal disorders.
Treatment options for achalasia aim to alleviate symptoms by reducing pressure at the LES and facilitating the passage of food into the stomach. This may include pneumatic dilation, a procedure in which a balloon is inflated within the LES to stretch and disrupt muscle fibers, or surgical myotomy, where the muscles of the LES are surgically cut to relieve obstruction. Botulinum toxin injections into the LES may provide temporary relief of symptoms but are less commonly used due to the risk of side effects and the need for repeat injections. Dietary modifications, such as consuming softer foods and avoiding large meals, can also help manage symptoms associated with achalasia.
In conclusion, Gastroesophageal Reflux Disease (GERD), Hiatal Hernia, and Achalasia Cardia are three distinct yet interconnected esophageal disorders that can significantly impact an individual's health and well-being. Early recognition, accurate diagnosis, and appropriate management are essential in alleviating symptoms, preventing complications, and improving quality of life for those affected by these conditions.
