A hiatal hernia is a medical condition characterized by the protrusion of part of the stomach through the diaphragm into the chest cavity. This condition can be categorized into two main types: sliding hiatal hernia and paraesophageal hiatal hernia.
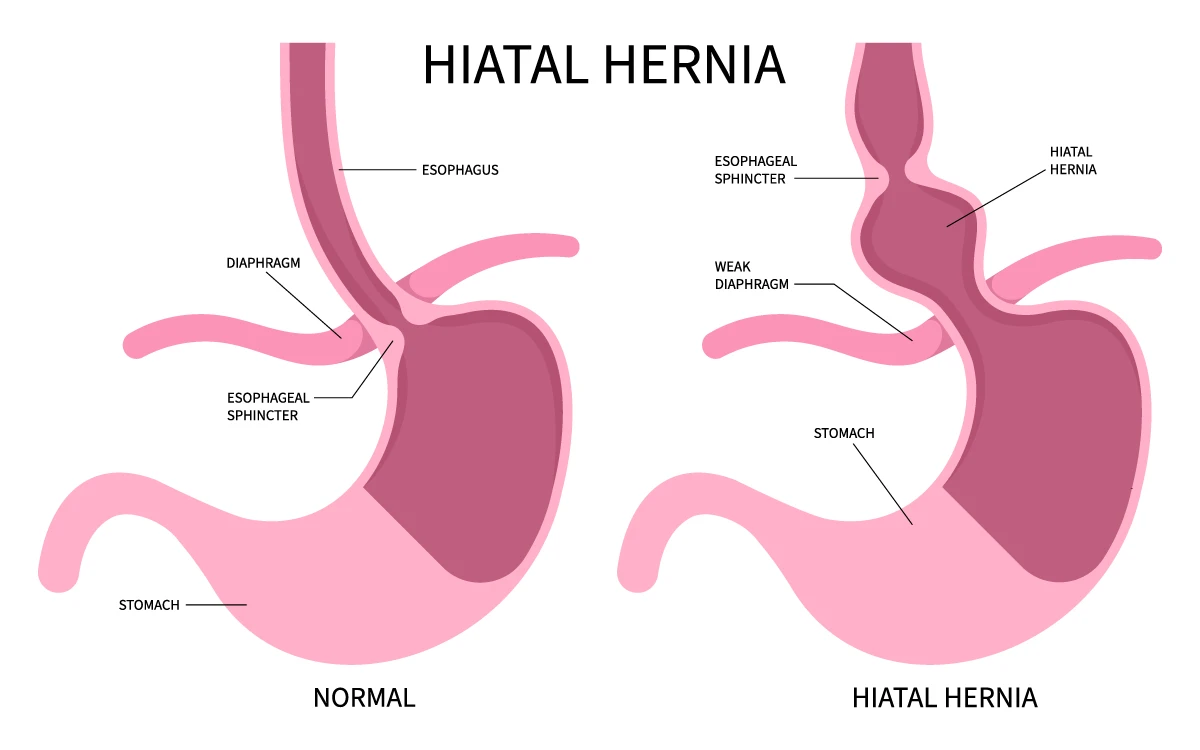
In a sliding hiatal hernia, the gastroesophageal junction and the upper part of the stomach slide up into the chest through the esophageal hiatus, which is an opening in the diaphragm that allows the esophagus to pass through to the stomach. This type of hernia is more common and usually does not cause symptoms. However, it can sometimes lead to gastroesophageal reflux disease (GERD) due to the displacement of the lower esophageal sphincter, which can result in heartburn, regurgitation, and other symptoms of GERD.
On the other hand, a paraesophageal hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm alongside the esophagus, while the gastroesophageal junction remains in its normal position. This type of hernia can be more concerning as it may cause complications such as gastric volvulus, where the stomach twists upon itself, leading to obstruction and potential strangulation of the blood supply to the stomach.
The exact cause of hiatal hernias is not always clear, but several factors may contribute to their development. These include weakening of the diaphragm muscles, increased pressure in the abdomen due to factors such as obesity, pregnancy, or heavy lifting, and age-related changes in the connective tissues supporting the diaphragm.
Symptoms of a hiatal hernia can vary widely depending on the type and severity of the hernia. In some cases, individuals may experience no symptoms at all, especially if they have a small sliding hiatal hernia. However, larger hernias or paraesophageal hernias may cause symptoms such as heartburn, chest pain, difficulty swallowing (dysphagia), belching, regurgitation of food or liquid, feeling full quickly after eating (early satiety), and shortness of breath.
Diagnosis of hiatal hernia typically involves a combination of medical history, physical examination, and diagnostic tests. Imaging studies such as X-rays, barium swallow studies, or endoscopy may be performed to visualize the hernia and assess its size and extent. Additionally, tests such as esophageal manometry and pH monitoring may be conducted to evaluate the function of the esophagus and determine the presence of GERD.
Treatment of hiatal hernia depends on the severity of symptoms and the presence of complications. In many cases, lifestyle modifications and medications can help manage symptoms of GERD associated with hiatal hernias. These may include avoiding large meals, acidic or spicy foods, caffeine, alcohol, and tobacco, as well as elevating the head of the bed and maintaining a healthy weight. Medications such as antacids, H2 receptor antagonists, or proton pump inhibitors (PPIs) may be prescribed to reduce acid production and alleviate symptoms.
In cases where lifestyle modifications and medications are ineffective or complications arise, surgical intervention may be necessary. Surgical options for hiatal hernia repair include laparoscopic (minimally invasive) procedures such as Nissen fundoplication, which involves wrapping the top of the stomach around the lower esophagus to reinforce the lower esophageal sphincter and prevent reflux, or hernia repair with mesh reinforcement in cases of paraesophageal hernias.
Overall, hiatal hernias are common conditions that can range from asymptomatic to potentially serious. Early diagnosis and appropriate management are essential in preventing complications and improving quality of life for affected individuals.
