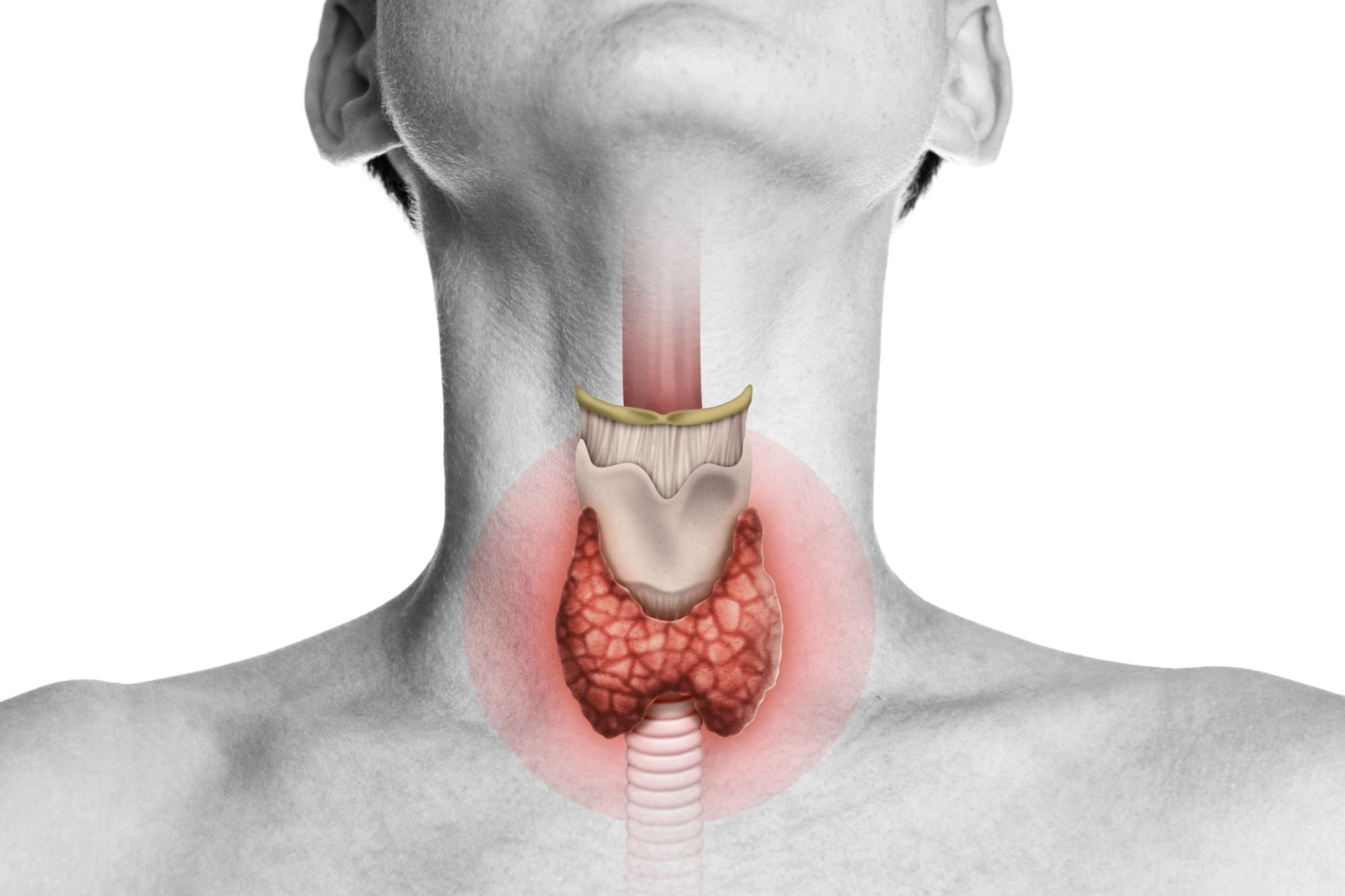
Thyroid surgery, also known as thyroidectomy, is a medical procedure performed to address various conditions affecting the thyroid gland. The thyroid gland, situated in the neck, plays a crucial role in regulating metabolism and producing hormones that influence numerous bodily functions.
There are several reasons why a thyroid surgery may be recommended:
1. Thyroid Cancer
Thyroid cancer occurs when abnormal cells in the thyroid gland grow uncontrollably. Surgery is often the primary treatment for thyroid cancer, aiming to remove the cancerous tissue and possibly surrounding lymph nodes to prevent further spread.
2. Thyroid Nodules:
Thyroid nodules are growths or lumps that form within the thyroid gland. While most nodules are benign, some may be cancerous or cause symptoms such as difficulty swallowing or breathing. Surgery may be necessary to remove nodules that are suspicious for cancer or causing significant symptoms.
3. Hyperthyroidism:
Hyperthyroidism is a condition characterized by an overactive thyroid gland, leading to excessive production of thyroid hormones. In cases where medication or other treatments fail to control symptoms, surgical removal of part or all of the thyroid gland (subtotal or total thyroidectomy) may be recommended to normalize hormone levels.
4. Goiter:
A goiter is an enlargement of the thyroid gland, often resulting from iodine deficiency, autoimmune diseases, or thyroid nodules. Surgery may be required to remove the goiter if it causes symptoms such as difficulty swallowing, breathing, or speaking, or if it is cosmetically bothersome.
Before undergoing thyroid surgery, patients typically undergo thorough evaluation, including medical history review, physical examination, blood tests, and imaging studies such as ultrasound or CT scan. This evaluation helps determine the type and extent of surgery needed and assesses the patient's overall health and potential risks.
Thyroid surgery can be performed using different techniques, depending on the specific condition and patient factors:
Conventional Thyroidectomy:
In a conventional thyroidectomy, an incision is made in the front of the neck, and the thyroid gland is carefully dissected and removed. This approach provides direct access to the thyroid gland and allows the surgeon to visualize surrounding structures.
Minimally Invasive Thyroidectomy:
Minimally invasive techniques, such as endoscopic or robotic-assisted thyroidectomy, involve smaller incisions and specialized instruments to access and remove the thyroid gland. These techniques may result in less visible scarring and potentially faster recovery compared to conventional surgery.
During the surgery, the surgeon takes care to preserve structures surrounding the thyroid gland, such as the parathyroid glands (which regulate calcium levels) and the recurrent laryngeal nerves (which control vocal cord function), to minimize the risk of complications such as hypoparathyroidism or vocal cord paralysis.
After the surgery, patients are closely monitored for any complications such as bleeding, infection, or changes in voice or calcium levels. Most patients can resume normal activities within a few weeks, although full recovery may take longer. Thyroid hormone replacement therapy is often necessary after total thyroidectomy to maintain hormonal balance.
In conclusion, thyroid surgery is a vital intervention for various thyroid conditions, including cancer, nodules, and hyperthyroidism. It aims to remove diseased tissue, alleviate symptoms, and restore thyroid function, ultimately improving patients' overall health and quality of life.
