A hiatal hernia is a medical condition characterized by the protrusion of part of the stomach through the diaphragm into the chest cavity. This condition can be categorized into two main types: sliding hiatal hernia and paraesophageal hiatal hernia.
A rare hernia, though less common than its more prevalent counterparts, presents unique challenges and considerations in both diagnosis and treatment. This condition occurs when abdominal organs protrude through an abnormal opening in the abdominal wall, leading to potential complications and discomfort for the affected individual.
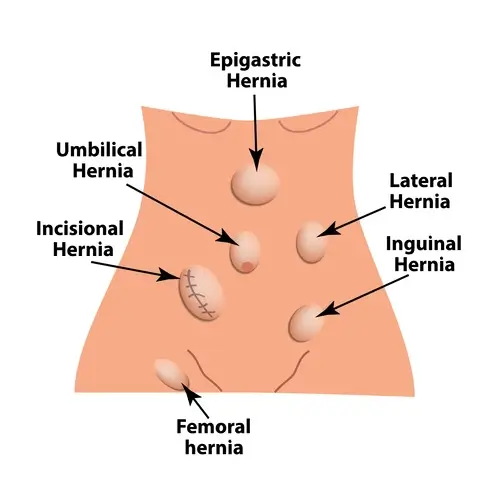
The term "hernia" itself refers to the protrusion of an organ or tissue through an opening or weak spot in the surrounding muscle or connective tissue. While inguinal and umbilical hernias are among the most frequently encountered types, rare hernias encompass a spectrum of less common variants that can affect various areas of the body.
One such example is the obturator hernia, which occurs when abdominal contents, typically the small intestine, protrude through the obturator canal—a narrow passageway in the pelvis. This type of hernia is particularly rare and is more commonly seen in elderly women with a history of pelvic surgery or significant weight loss. Due to its location deep within the pelvis, obturator hernias can be challenging to diagnose and may present with vague symptoms such as groin or thigh pain.
Another uncommon hernia type is the lumbar hernia, where abdominal contents herniate through defects in the lumbar region of the back. These hernias can be congenital or acquired, with acquired lumbar hernias often occurring secondary to trauma or previous surgery in the area. While lumbar hernias are rare, they can lead to significant complications such as bowel obstruction or strangulation if left untreated.
Other examples of rare hernias include diaphragmatic hernias, which involve the protrusion of abdominal organs into the chest cavity through defects in the diaphragm, and sciatic hernias, where abdominal contents herniate through the sciatic foramen—a passageway in the pelvis. These types of hernias are relatively uncommon and may present with atypical symptoms that can make diagnosis challenging for healthcare providers.
Diagnosing rare hernias often requires a combination of clinical evaluation, imaging studies, and sometimes, invasive procedures such as laparoscopy or exploratory surgery. Healthcare providers must maintain a high index of suspicion for these conditions, especially in patients with nonspecific abdominal or pelvic symptoms and a history of risk factors such as previous surgeries or trauma.
Treatment of rare hernias typically involves surgical intervention to repair the underlying defect and reduce the risk of complications. However, due to the complexity and rarity of these hernia types, surgical management may require specialized expertise and techniques. In some cases, minimally invasive approaches such as laparoscopy or robotic-assisted surgery may be employed to repair the hernia while minimizing postoperative morbidity.
Despite advancements in surgical techniques and perioperative care, rare hernias can pose significant challenges for both patients and healthcare providers. Complications such as bowel obstruction, strangulation, or recurrence may occur, highlighting the importance of timely diagnosis and appropriate management. Additionally, rare hernias may be associated with underlying anatomical abnormalities or systemic conditions that warrant further evaluation and management.
In conclusion, rare hernias encompass a diverse array of less common variants that present unique challenges in diagnosis and treatment. Healthcare providers must maintain awareness of these conditions and consider them in the differential diagnosis of patients with abdominal or pelvic symptoms. Through a multidisciplinary approach involving clinical evaluation, imaging studies, and surgical expertise, patients with rare hernias can receive timely and effective management to optimize outcomes and minimize complications.
