A ventral hernia is a condition characterized by the protrusion of abdominal organs or tissue through a weakened area in the abdominal wall. This type of hernia occurs in the anterior abdominal wall, hence the term "ventral."
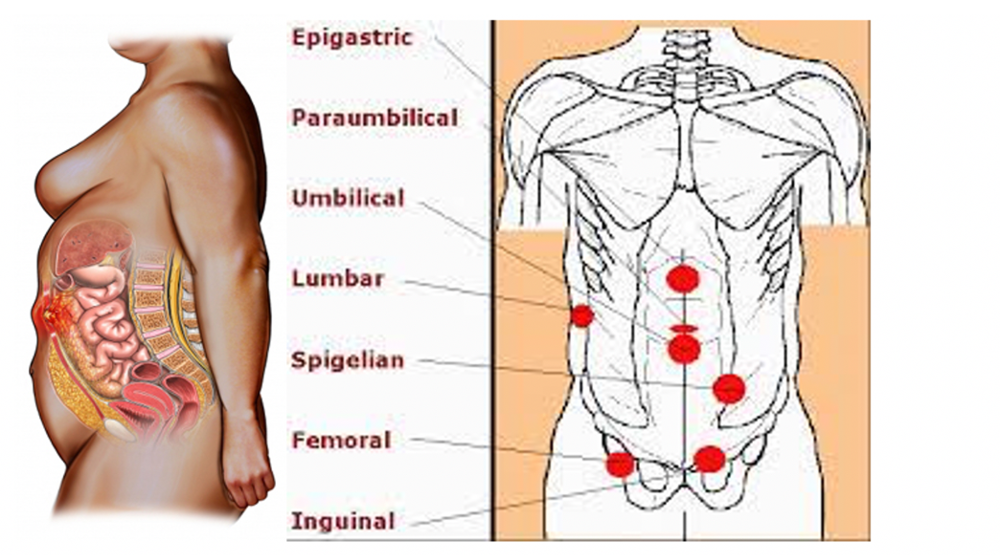
To understand ventral hernias better, it's essential to grasp the anatomy of the abdomen. The abdominal wall is composed of several layers of muscle and tissue that help protect the organs within the abdominal cavity. These layers include the skin, subcutaneous fat, muscles (such as the rectus abdominis, internal oblique, and external oblique), and connective tissue.
Under normal circumstances, the abdominal wall is strong and resilient, providing support and protection to the abdominal organs. However, certain factors can weaken this wall, making it susceptible to herniation. These factors may include:
1. Surgery:
Previous abdominal surgeries, particularly those that require incisions in the abdominal wall, can weaken the tissue and increase the risk of herniation.
2. Trauma:
Blunt force trauma or injury to the abdomen can damage the muscles and tissue, creating weak spots where hernias can develop.
3. Obesity:
Excess body weight can exert pressure on the abdominal wall, leading to muscle weakness and an increased risk of herniation.
4. Pregnancy:
The stretching of the abdominal muscles and tissue during pregnancy can weaken the abdominal wall, predisposing women to develop ventral hernias, especially after childbirth.
5. Aging:
As people age, their muscles and connective tissue may weaken, making them more susceptible to hernias.
6. Chronic coughing or straining::
Conditions such as chronic obstructive pulmonary disease (COPD) or constipation can lead to repetitive straining, which puts pressure on the abdominal wall and increases the risk of herniation.
When a ventral hernia occurs, it typically presents as a visible bulge or lump in the abdomen. The size and location of the hernia can vary, ranging from small and asymptomatic to large and symptomatic. Common symptoms of ventral hernias may include:
- A visible bulge or lump in the abdomen, particularly when standing, coughing, or straining.
- Pain or discomfort at the site of the hernia, which may worsen with activity or when lifting heavy objects.
- Nausea, vomiting, or constipation if the hernia becomes incarcerated or strangulated (the herniated tissue becomes trapped and loses its blood supply).
Diagnosis of ventral hernias typically involves a physical examination by a healthcare provider. In some cases, imaging tests such as ultrasound, CT scan, or MRI may be ordered to confirm the diagnosis and assess the size and extent of the hernia.
Treatment options for ventral hernias depend on several factors, including the size and location of the hernia, as well as the presence of symptoms. In many cases, small asymptomatic hernias may be managed conservatively with watchful waiting and lifestyle modifications, such as weight loss and avoiding heavy lifting. However, larger or symptomatic hernias often require surgical repair to prevent complications such as incarceration or strangulation.
Surgical repair of ventral hernias may be performed using open or minimally invasive techniques. During the procedure, the protruding tissue is pushed back into place, and the weakened area of the abdominal wall is reinforced with sutures or a synthetic mesh to provide additional support. The type of surgical approach and technique used will depend on individual patient factors and the preferences of the surgeon.
Recovery from ventral hernia repair surgery varies depending on the extent of the procedure and individual factors such as overall health and fitness level. Most patients can expect to resume normal activities gradually within a few weeks following surgery, although heavy lifting and strenuous exercise may need to be avoided for a longer period.
In conclusion, ventral hernias are a common condition characterized by the protrusion of abdominal organs or tissue through a weakened area in the abdominal wall. While small hernias may be managed conservatively, larger or symptomatic hernias often require surgical repair to prevent complications and improve quality of life. Early diagnosis and appropriate treatment are essential for minimizing the risk of complications and achieving optimal outcomes for patients with ventral hernias.
